Public Sector Collaboration: Building a Healthier, More Connected Future
The recent change in government, coupled with new investments in the NHS from the 2024 October budget, has brought a renewed sense of opportunity for healthcare, social care, and local government leaders. The ongoing change consultation by the Department of Health and Social Care (DHSC) further highlights the importance of rethinking our approach to system-wide collaboration. For leaders across the North West, this is a pivotal moment to champion partnerships, foster grassroots engagement, and embed systems working as the foundation for sustainable change.
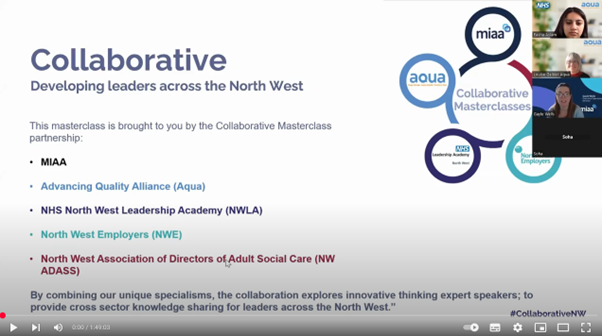
At the North West Learning and Development Collaborative, a partnership encompassing North West Employers, the NHS North West Leadership Academy, the NHS Clinical Leadership Network (NHS CLN), Health Innovation North West Coast, AQUA, and MIAA, we believe that collaborative working is the cornerstone of building resilient public services.

The Case for Collaboration in Public Services
Public sector challenges, including health inequalities, workforce shortages, and financial pressures, require a joined-up approach. The NHS and local government are not just service providers but anchors in their communities, with an ability to shape lives and drive regional growth. Siloed decision-making leads to inefficiencies and fragmented care, we need to be breaking down barriers between organisations to deliver better outcomes.
Key Themes for Leaders to Enable Collaboration
Fostering Grassroots Engagement
Change cannot be imposed from the top; it must be co-created with those it affects most. Invest in listening exercises to understand the unique needs of local populations and frontline teams. Facilitate co-design workshops to empower staff and communities. Promote open communication channels to capture feedback and ideas continuously.
A compelling example of this approach in action is NHS Cheshire and Merseyside ICS’s addressing of fuel poverty, a rapidly growing problem particularly impacting people with respiratory conditions. The ambition of this project was to ensure all stakeholders from across the ICS were working collaboratively to find and deliver solutions that would lessen the impact of fuel poverty on the health of the population who are most affected.
A fuel poverty dashboard was developed within the CIPHA (Combined Intelligence for Population Health Action) data system. This identifies the population cohorts at greatest risk of harm by bringing together several datasets, including primary care patient-level data, SUS data, local feeds from providers (e.g., pregnancy register), ONS – fuel poverty by Lower Layer Super Output Areas (LSOA), and Ministry of Housing, Communities, and Local Government energy efficiency data.
Optum facilitated system-wide workshops, where two distinct target cohorts were selected from the most fuel-poor neighbourhoods: adults with severe COPD and children with early signs of asthma. Following this case-finding, unique population health management (PHM) approach-themed solutions, including the payment of fuel bills and holistic lifestyle reviews, were carried out. The aim was to improve the respiratory health of these populations, ensuring they could afford to heat their homes safely and reduce their utilisation of NHS services. Initial patient interviews have reported that patients are using less primary and secondary care following their interventions.
Pathways were deployed in four places during phase 1 of the work in 2023/24. These areas are continuing to deliver during phase 2, and there are four new areas due to go live in Q4 24/25. This project has started to narrow health inequalities by linking data, but more importantly, by linking people.
The University of Liverpool is involved in the evaluation. They have identified matched cohorts in CIPHA to compare our patient cohorts with others that haven’t been supported. This only started recently, as we needed a minimum number of patients to have been on the pathway for six months. Initial findings indicate a reduction in the number of presentations at A&E and admissions to secondary care.
Highlights to date:
- Almost 650 patients were identified and put on the pathway
- Over 500 people had their medicines optimised
- Facilitated £362,000 payments from local authority household support fund
- Over 500 referrals to local authority commissioned affordable warmth schemes
- 325 referrals to wellbeing and social prescribing teams
- Over 270 families added to the priority services register with energy providers
Grassroots engagement ensures that frontline staff, patients, carers, and communities have a voice in shaping services.
Building Partnerships Across Sectors
True collaboration means going beyond organisational boundaries. Local authorities, healthcare providers, voluntary organisations, and private sector partners all have a role to play in creating integrated care systems (ICSs).
In 2017 local response to the scale and complexity of the health and social care challenge saw leaders from key organisations across St Helens come together in an innovative new configuration to form the “St Helens People’s Board”. This borough-based partnership included public, private and third-sector organisations, some of which are not typically involved in the provision of health and care such as housing and blue light services.

Their approach was underpinned by a commitment to untangle the complex interplay between wider determinants of health and wellbeing. Members of the Board worked to establish a shared vision and responsibility to manage demand; reduce costs and improve local health and care outcomes through setting up an integrated care system entitled “St Helens Cares” (SHC). To read more about this project click here.
Some key takeaways from this example are:
- Establish joint accountability and collaborative structures that balance project delivery and flexibility.
- Invest in technical solutions for sharing information across organisational boundaries.
- Share data, insights, and resources to drive quality improvement and learning.
Leaders should champion shared goals and metrics that reflect collective success.
Strengthening Workforce Resilience
The public sector workforce is the backbone of our services. Supporting wellbeing and development is key to achieving sustainable systems working.
The North West Learning and Development Collaborative advocates investing in workforce development as a foundation for thriving local economies and strongly recommends organisations.
Prioritise staff wellbeing by embedding mental health support and flexible working policies.

In 2024 three public sector partner organisations; Northern Care Alliance, Tameside and Glossip Integrated Care NHSFT and UNISON spearheaded the adoption of a new well-being and attendance management policy, coproduced between a multi-agency staff community of practice, designed to focus on holistic wellbeing and reduce ineffective punitive triggers. This policy recognises that sickness rates in the North West have been the highest in the country for some time and current policies have not changed this and evidence suggests that current policy in fact has the opposite effect. This policy aims to use compassionate principles to improve staff wellbeing reducing sickness and absence rates and ultimately improving the quality of care delivered across the region. Guidance for other North West organisations looking to adopt this approach can be found here:
Wellbeing & Attendance Management Policy Implementation ToolkitEmbedding a Culture of Learning and Adaptation
Collaboration thrives in an environment where learning is continuous and innovation is encouraged. Leaders must create cultures that embrace experimentation and adaptation.
The North West Collaborative Masterclasses hosted by the North West Learning and Development Collaborative and ADASS are regular events that:
- Create safe spaces for staff to share and test new ideas and learn from failures.
- Showcase the examples of collaborative initiatives and their impact to the region.
- Promote knowledge-sharing networks to disseminate best practices across sectors.
You can find a list of upcoming masterclass sessions and recordings here:
Leveraging New Funding for Transformation
The additional NHS funding announced in the October 2024 budget presents an opportunity to invest in initiatives that support long-term collaboration such as:
- Align funding priorities with system-wide goals to maximise impact.
- Use funding to address systemic issues, such as digital infrastructure, which underpin collaborative working.
- Build capacity for preventative care to reduce demand for acute services.
A consortium of nine local authorities shared government ring-fenced funding to improve their in-patient (IPD) drug and alcohol detox treatment and recovery systems.
Funding is collectively managed and used to commission service providers through ‘block contract’ arrangements.
A new patient pathway designed by MIAA Solutions has seen seven new service providers commissioned through block contract arrangements via a single procurement approach, with the collective buying power of the consortium creating a ‘healthy’ bed night price competition. This has delivered significant savings for lower-funded authorities and increased service provider diversity through individual procurement processes.
Wider health system benefits have included a reduction in frequent presenter attendance in acute facilities, deaths in treatment and calls to support requirements from community providers.
The consortium is now piloting additional funding streams that will enable authorities, who have already spent their grant-funding allocation, the ability to make further referrals through the consortium pathway, delivering further improvements in patient outcomes.
To read more about this consortium click here:
Read moreLeading the Charge for Collaborative Futures
The UK’s changing political and financial landscape offers a unique opportunity for public sector leaders to reimagine how we work together.
The North West Learning and Development Collaborative represents the collaborative pooling of regional development resources into a better-for-all model. For more information on how the collaborative can support your organisation or system collectively contact